From Grangeville, Idaho, it's a one-hour-and-18-minute drive to the closest Walmart and a one-hour-and-18-minute drive back. This blip of a town along Highway 95 sits at the edge of national forest, somewhere between Lewiston and the middle of nowhere. Yet with just over 3,000 people, it's the largest city in the most spread-out county in the entire state.
Jennifer Griffis and her family live outside of Grangeville, in a green-roofed house with bikes scattered across the lawn. "Sometimes our cellphones work out here and sometimes they don't," she says.
Griffis, her husband and their seven children moved here in 2010, drawn by how close the mountains were. But when something went wrong with her daughter Monique, Griffis learned exactly how far away they really lived.

There are no licensed psychiatrists in private practice in Idaho County, nor in neighboring Lewis and Clearwater counties. Yet there was no question Monique needed help. She'd hurt people, then smile. In one episode, Griffis recalls Monique choking her 2-year-old sister in the backseat of their Suburban. "She looked at me with this very cold expression," Griffis says. "[She said]: 'I was trying to choke her. Because I wanted to kill her.'"
Eventually Monique was diagnosed with a conduct disorder with limited prosocial emotions. "No remorse," Griffis says. "No conscience, no empathy ability."
That disorder has meant a 140-mile round trip to Lewiston to visit a psychologist. It's meant driving back from Boise in a blizzard after visiting Monique in therapeutic foster care. It's meant five-hour trips back and forth to a treatment facility in Helena, Mont., with the whole family packed into the SUV.
"There are absolutely no residential treatment facilities for females under the age of 12 in Idaho," Griffis says.
Rural communities are never going to have every kind of doctor. But in Idaho, the problem is compounded: The state is rural and underfunded, with a high incidence of mental illness.
Despite its sky-high suicide rates, it was the last state in the nation to get a suicide hotline.
"The number of holes that are occurring in Idaho has been getting progressively larger," says Casey Moyer, a program manager with Idaho's Health and Welfare department.
With a third of its population living out in the country, Idaho ranks with Montana among America's most rural states — and every Idaho county has a mental health care provider shortage. Analysis by the nonprofit Mountain States Group shows that a quarter of Idaho's population lacks access to a psychologist or psychiatrist.

The state is last in the number of psychiatrists per person, according to 2012 Kaiser Family Foundation data. It also ranks last in mental health funding (though Idaho officials claim that ranking is skewed because it doesn't include Idaho's Medicaid spending).
"I'm trying to think of anything they do well, actually," says Kathie Garrett, board member of the Idaho chapter of the National Alliance on Mental Illness and a former state representative from Boise. "We do very little on the front end. All our state-funded services are for those in crisis, who are a danger to themselves and others."
On a sliver of a budget, Idaho is trying to change that, shifting its entire mental health care model and searching for ways to bring help to the farthest reaches of the state.
But to get there, it has a very long way to go.
Roadblocks
It's Tuesday evening at the Snake River Community Clinic in Lewiston. The clinic helps patients with both mental and physical problems, but today, a full two-thirds of the patients are suffering from depression. A few have anxiety. Clinic staff helps one woman — suffering from post-traumatic stress disorder after domestic violence — sneak out the back door.
"Over 30 percent of our patients come here for mental health because they can't go anywhere else," says clinic director Charlotte Ash.
Nearly 1,750 different patients have come to the clinic over the past year. They drive from hundreds of miles away, from tiny towns like Riggins and Weippe and Enterprise, from at least five counties in Idaho, two in Washington and one in Oregon.
The rural counties in Idaho's lower panhandle are among the state's poorest, but at the Snake River clinic, there's no sliding scale, no messing with insurance. If you can get in, it's free. But getting there isn't.
"A lot of our patients have to decide: Are they going to spend the money on gas to get here and get help, or are they going to get groceries?" Ash says.
The clinic sometimes mails out medications when clients can't get to appointments. Other times, Ash gives patients a $20 bill for gas to get home. One state clinician says he's personally driven clients down from Moscow in his state-provided Chevy.
There are other barriers: Sometimes the roads themselves are hard to traverse. One 2010 study called Idaho's roads the second-worst-maintained in the nation.
"A lot of these patients live in these extra-rural wilderness areas," says Fayth Dickenson, a clinical care manager at St. Joseph Regional Medical Center in Lewiston. "They're on top of a mountain, [at the end] of a one-way dirt road. They call, and can't leave their house because their roads are snowed in."
In Boundary County, at the very top of the Idaho panhandle, a zoning ordinance warns prospective property owners of rugged living where "snows often knock out power, sometimes for days or weeks on end, and roads are often rendered impassable by snow or by flooding in the spring when the snow melts."
Bonners Ferry resident Jini Woodward knows that county and its mental health system well. Her daughter, now 45, has dealt with severe anxiety and mood disorders for more than two decades.
"Because there weren't enough services, her illness progressed," Woodward says. "Boundary County has to depend on Bonner County, and Bonner County has to depend on Kootenai County. The services are so inadequate in Kootenai County. And we're clear at the end of the road; we're the last hair on the tail."
Without enough services in Bonners Ferry, Woodward's mentally ill daughter decided to move to Sandpoint. There weren't enough services there either, so she moved to Hayden. That's put her hours away from her parents.
"We rely on telephones and emails to keep in touch," says Woodward, who's considering moving to Sandpoint herself. "It's a lot harder to monitor her situation."
Social stigma around mental health can be another obstacle to care, especially in smaller towns. But some providers are now moving toward combining medical and mental health services.
At a clinic on the sprawling Nez Perce Indian Reservation, patients may come in with coughs, but a doctor might also tell them they've scored high on a certain depression measure. It may be their only chance to talk.
"When I see a patient, it may be the first and last time I see the patient," says Kristy Kuehfuss, Nimiipuu Health's director of behavioral health.
That means Kuehfuss may have to streamline months of therapy — diagnosing and educating the patient — in less than an hour. She concentrates on immediate practical tips, such as encouraging depressed patients to get out of bed and go outside every day.
Kuehfuss says living rurally carries additional psychological costs. "For somebody who already has a mental health disorder, anxiety and depression," she says, "it's going to be exacerbated by the physical and social isolation."
I.T. help
In a clinic in Cottonwood, Idaho, a child and parent talk with psychiatrist William Terry. They may talk about bipolar disorder, attention-deficit disorder or abuse, discussing how well their medication is working. It's a typical conversation in almost every way but one: The kid and his parents are talking to a head on a high-definition screen hanging from a robot called the RP-Lite. The RP-Lite looks less like C-3PO and more like a coat rack with a face attached to the end.
Terry is 200 miles away, at a dual-screen terminal at Saint Alphonsus Regional Medical Center in Boise. Using the joystick, he swings the robot's head and the video screen side to side. He can zoom in to observe a patient's tremors or tics.
"You can move the camera so that we can focus in on the people's face," Terry says. "If they're around the room, I can follow them in the room." It only takes seconds for the distance to fade away, and for it to feel almost like any in-person session.

"One of the kids that has been seen by the psychiatrist saw the robot in the hallway," recalls Pam McBride, special assistant to the president of St. Mary's/Clearwater Valley Hospital and clinics. "The kiddo just ran up to it and hugged the robot and said, 'Hi, Dr. Terry!'"
St. Mary's Hospital in Cottonwood and Clearwater Valley Hospital in Orofino are in areas defined as "frontier"— the most rural of the rural. Psychiatric help for children is at least three hours away.
"Over 80 percent of the patients who took advantage of telepsychiatry services had never seen a psychiatrist before," says McBride. "They had no access."
When the first robots rolled into the two hospitals back in 2009, isolated communities were connected with psychiatric care for the first time. And it worked. A nonscientific examination of their data indicated a dramatic decline in primary care doctor, emergency room and hospital visits among those who'd conducted long-distance sessions with the psychiatrist.
In other words, it was not only helping patients — it was driving down costs for the entire system.
"We've seen kids go from almost getting kicked out of schools, because of behaviors that are out of control, to becoming Student of the Month," McBride says.
In study after study analyzing Idaho's mental health system, "telepsychiatry" continues to come up as one piece of the solution. The St. Mary's hospital system wants to go further, using cheaper and more conventional video-chat technology to provide psychiatric help to even more far-flung clinics.
"Patients adapt to it much easier than health care providers do," says psychiatrist William Hazle. "Think of how much time we spend watching the television screen. Now we talk to it."
While telepsychiatry can bring help to remote locations, it doesn't fix the fact that psychiatrists are in short supply everywhere in Idaho, even in Boise. Not all of them are comfortable conducting therapy sessions over video screen.
"Doctors weren't trained to practice this way. You have to have a certain kind of doctor who's willing to try this method," McBride says. "They're used to having someone in front of them."
Last year, Idaho doctor-turned-legislator Rep. John Rusche launched the Idaho Telehealth Task Force, which recently applied for a $2.3 million grant to train doctors and encourage providers to adopt telemedicine technology. Over three years, the Task Force estimates the state could save $19.3 million.
Yet there are places like St. Joseph Regional Medical Center, which once used telepsychiatry but longer do. The program ended when the provider left the practice. That's the challenge with any rural innovation: Not just attracting the right talent, resources and programs — but keeping them.
The cost of cuts
Nuclear engineer Ryan Mitchell had never heard the name Gerald Durk Simpson before Simpson shot him in the back.
Mitchell only happened to be at Mocha Madness in Pocatello on that day in September 2010 because he didn't have Internet access at his apartment.
He was a few steps outside the coffee shop when Simpson, a schizophrenic 54-year-old, shot him point-blank. The bullet went through his back, through his left lung and embedded itself in his sternum. It missed the heart chamber by about an inch.
"Ryan won't ever fully recover," says his father, Robert. "The scar went from his spinal cord almost to his sternum. He'll always have some deformity. He has permanent nerve damage. His scapula is detached."
Statistically, mental illness rarely results in violence. But when it does, it thrusts the issue into the public eye.
"It's not like we wanted to become the poster children for mental health care in Idaho, but we kind of became that," Robert Mitchell says.
Idaho's Health and Welfare department is intended to fill a gap, providing mental health care for those without access to insurance or Medicaid. To balance the budget, Idaho eliminated redundancy. In the summer of 2010, 451 mentally ill Idahoans were kicked off state coverage and onto Medicaid or private insurance.
Simpson was among 70 Pocatello-area residents who'd been dropped from a state-funded, community-based treatment program that assisted them in living independently.
A month after the shooting, Ryan Mitchell attended a political candidates' public forum in downtown Pocatello and asked a pointed question about why he got shot.
"The fact of the matter is this was caused by recent budget cuts to our mental health program," he said. "My question is ... What are you going to do to fix it?"
Two years later, the charges against Simpson were dismissed after a magistrate determined he lacked the mental capacity to stand trial. During those two years, Mitchell and his parents' plea for more mental health care funding went unfulfilled: An additional $1.85 million was cut from the state's mental health budget.
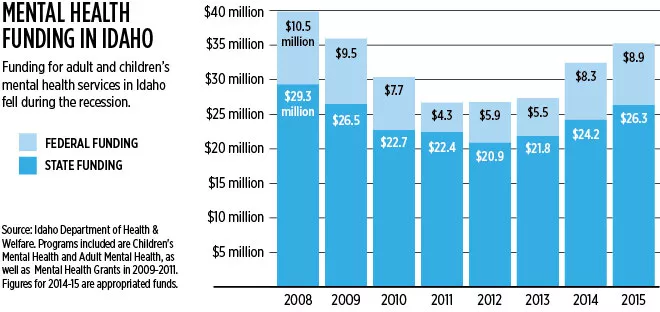
The recession devastated Idaho's mental health care system in a way it still hasn't recovered from. From 2008 to 2012, state funding fell by more than 28 percent. During that same period, federal funding collapsed nearly by half.
The cuts gouged deep through Idaho. In 2010, Health and Welfare eliminated 126 positions statewide and shuttered nine rural offices.
"We made it a goal to not stop serving people," says Ross Edmunds, administrator of the department's Behavioral Health division. When the offices closed, the department continued working through local clinics. The state served more patients total, yet had to dramatically cut back on the breadth of services.
For patients who aren't suicidal or homicidal, the state has stopped providing psychotherapy and case-management services.
Of course, in the midst of all this, Idaho had an option to give vastly more people mental health care, while saving the cash-strapped state more than $400 million across 10 years, according to a report from the Idaho Workgroup on Medicaid Expansion. It just had to expand Medicaid under the Affordable Care Act.
Initially, the federal government would pay the entire bill. But Idaho Gov. Butch Otter, like most Republican governors, rejected the offer, arguing that Medicaid should be reformed first.
The bright side
In fact, reform is happening. An in-depth 2008 report called Idaho's mental health system "severely fragmented, with a significant lack of clarity." It proposed solutions, like combining mental health and substance abuse departments. Now, Idaho has done just that.
It's also handed state regional mental health boards a little more power. "Previously they were only an advisory group. They couldn't have their own budget or own staff. They couldn't apply for grants. Nothing," Edmunds says.
On July 1, the old regional mental health boards will disappear, replaced by behavioral health boards that focus on mental health and drug abuse. Each of the seven regions will have a small $45,000 budget, be able to hire staff members and apply for their own grants. The boards know their communities, the thinking goes. They know where resources are most needed.
That's far from the biggest change. In September, Idaho switched from a fee-for-service model for Medicaid to a "managed care" model, run by a national organization called Optum. Instead of the health care business model that profits more the longer patients are sick, managed care organizations have financial rewards for getting people healthy quickly. They strictly monitor the cost and effectiveness of treatments. "The impact of that is tremendous," Edmunds says.
In Grangeville, Griffis has been impressed. "They handled our very complex situation well," she says. "We were able to get some answers to questions before I even needed to ask."
Yet reviews have been far from universally positive. Some providers see Optum as another layer of red tape: more paperwork, more restrictions, less time with patients.
"We used to be able to do 60-minute sessions," says Jenny Brotherton-Manna, who runs North Idaho Children's Mental Health in Sandpoint. Now most sessions are limited to 45 minutes. She now has to ask for permission to give patients certain treatments, and getting it sometimes means waiting two or three days.
And since she's only a therapist, there are now some practices Medicaid under Optum won't pay for at all.
"Medicaid has now stopped the payment of all testing to be done by masters-level therapists. I cannot get reimbursed," she says. "It has to be referred on to a psychologist or psychiatrist." Nearly half the counties in Idaho, according to the Mountain States Group, have neither. She says there's now an unprecedented four-month-long wait in her region for kids to see a neuropsychologist.
"I want to be able to provide the type of service [a patient] needs at that moment, without having to make two or three phone calls a day to get him some services," she says.
Optum has been given another huge responsibility: Fix rural access issues. Their contract demands there be at least one mental health care provider located within 45 miles or 45 minutes of any Idaho residence. In more densely populated counties, like Kootenai and Ada, the requirement is even stricter: 30 minutes or miles or less. If not, Optum is contractually bound to come up with a plan to fix it.
There's more good news: The budget stopped plummeting. Since last year, the state of Idaho has slowly been restoring mental health funding, though even by 2015, it will still fall short of pre-recession levels.
In this past legislative session, Health and Welfare asked for funding to add three new behavioral health crisis centers. One would be in Boise, another in Idaho Falls, and another in Coeur d'Alene.
The legislature came through — but only partially. "The legislature has only funded one of those facilities. It's embarrassing," Robert Mitchell says. "At least that's progress."
Right now, Coeur d'Alene is intensely competing with the biggest cities in eastern and southern Idaho for the clinic. Kootenai County's sheriff and four regional police chiefs signed a letter to state Sen. John Goedde last month, urging the state to pick Coeur d'Alene.
"Kootenai County has one of the highest suicide rates in the state," says Claudia Miewald, director of the Kootenai Behavioral Health Center. "We desperately need this in our community."
Staying put
Activists have called for more psychiatrists in Idaho, more telemedicine, more funding, more coordination and support. But change is slow, and many families of the mentally ill living in rural Idaho have had to consider another solution: packing up and finding somewhere else to live.
"We were told by two different people early on: 'If you were going to be dealing with this, Idaho is not where you're going to be,'" Griffis says. "There were times that we wondered if we needed to move."
But she feels like she has a responsibility to stay, to change Idaho instead of leaving Idaho. Today, she's on the State Planning Council on Mental Health. She urges the state to concentrate more on children's mental health, respite care and day-treatment centers to give parents a break.
"We feel like we're in a position to push for mental health services," Griffis says. "It will take some time to see where that goes. It takes people willing to speak out." ♦
Stopping Suicide
The correlation is undeniable: State by state, population density is one of the strongest predictors of suicide. All that loneliness, that isolation, that proud individualism that makes asking for help difficult adds up. Another major driver: access to firearms, which are used in more than half of Idaho's suicides.
The state is sixth in the nation when it comes to suicide rate, according to 2010 data from the Centers for Disease Control. Nearby Montana ranked third.
Yet for years, Idaho was the only state without a suicide hotline. That finally changed in November 2012. The state amassed enough funding to reopen the Idaho Suicide Prevention Hotline, which went dark in 2006 due to budget cuts.
"I think it's too early to tell if there's been an impact," says John Reusser, the hotline's director. "Anecdotally, I can say we've saved lives."
Last year, nearly 1,000 Idahoans — including 120 military members — dialed 1-800-273-8255 to receive counseling from a team of 43 volunteers manning the hotline. This year, the hotline has already received 752 calls. Follow-up calls have shown suicides have been prevented and callers have been connected with outside resources to help them get better.
Currently, those calling on weekends or between 1 and 9 am on weekdays have their calls answered by a network of volunteers from other states, but by the end of the year, Reusser says the Idaho hotline will operate 24/7.
Local volunteers are crucial. When callers call from Idaho towns like Filer or Coeur d'Alene, Reusser says, Idaho volunteers know exactly where they're calling from, and what rural life is like: "We understand what it's like to live here."
It's far from the only effort to stop suicide in Idaho. Last year, the Idaho Department of Education won a three-year grant for youth suicide prevention.