When it comes to dealing with chronic pain, one thing is becoming clearer and clearer: Opioids are not the answer.
Sure, opioids can provide quick relief for acute pain for the first couple weeks. But research shows that opioids for long-term use may not work at all in treating non-cancer chronic pain. That's without mentioning how opioid use is contributing to a pervasive drug epidemic in America.
But what's the alternative?
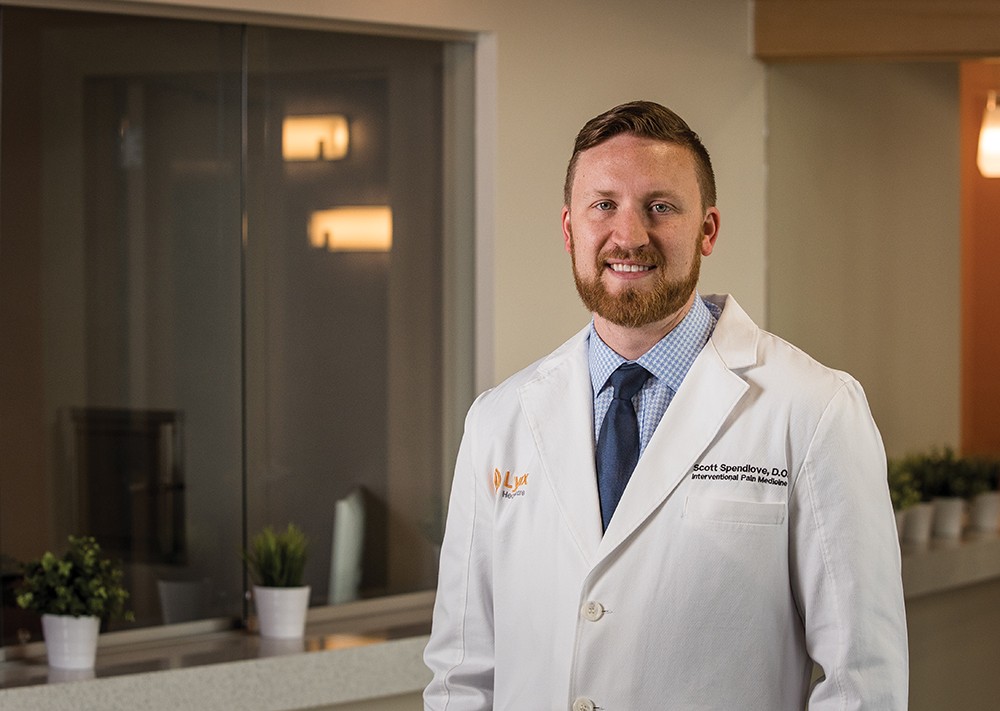
In fact, there are plenty of options, says Scott Spendlove, co-founder and chief medical officer of Lynx Healthcare, a local medical provider focusing on pain management.
As a teenager, Spendlove was diagnosed with ankylosing spondylitis, a type of arthritis that mostly affects the lower part of the spine. Even then, Spendlove knew opiates weren't the answer for his chronic pain.
"Ever since, I've had a passion and life vision of finding ways to treat chronic pain without opiates," Spendlove says.
At Lynx, Spendlove says they often see patients who have been on a high dose of opiates for 15-plus years, and yet they still experience pain, though sometimes, it actually improves when they are weaned off of the drug.
"Opiates in general are very ineffective at treating chronic pain," he says. "It's not a long-term treatment. It's not sustainable. It's one of the tools in the toolbox that is overutilized."
Instead, Spendlove offers a multidisciplinary approach to chronic pain.
It's a topic gaining more attention. People are becoming increasingly desperate for alternatives, says Marian Wilson, an assistant professor at Washington State University College of Nursing.
"Every pain is different," Wilson says. "There's a hundred different things people could try."
MOVING ON
It seems counterintuitive: When you feel like you're in too much pain to get up and move around, the best way to fight that pain is to, well, get up and move around.
"Through evolution, we have pain to tell us to stop," Spendlove says. "They feel that pain and they are automatically restricted and stop movements and assign themselves to the couch. But it's actually counterproductive."
To get moving, swimming and aqua therapy can be particularly effective, as can other forms of exercise and physical therapy. Spendlove says he tells patients to look up yoga on YouTube, or take a class if the structure will keep them motivated. Yoga's simple positions can be effective by helping to strengthen and lengthen muscles.
Strengthening exercises can also help, Spendlove says.
"The best back brace for your spine is a strong core," he says.
Sometimes even just going out for a walk or a bike ride can make a difference.
"I don't expect you to run a marathon tomorrow," he says. "Go out and enjoy the outdoors, and that will improve pain significantly."
Wilson says yoga and Tai Chi are two of the most highly studied physical forms of pain intervention, and she says there's plenty of research supporting them. They can especially help with muscular pain and fibromyalgia.
Yet it's not all physical. They can also help with the emotions of chronic pain. After all, it's hard not to feel discouraged if pain is a constant companion.
"Things like yoga and Tai Chi are not only working muscles building strength, but help with mood disorder," Wilson says.
MIND THE BRAIN
No, Spendlove tells patients. It's not "mumbo jumbo." Mindfulness and meditation techniques can be highly effective for pain management. At the very least, these techniques can help people not get as stressed out over the pain they're experiencing.
"What I try to get [patients] to wrap their minds around is that pain is a sensation that they themselves can turn the thermostat up on, and they can also turn that thermostat down," he says.
In other words, the more you focus and pay attention to the pain, the more prominent it becomes. Training your brain to not focus on it and to better manage the stress it produces can make a huge difference.
A more technical term for this is Cognitive Behavioral Therapy, or CBT. It includes addressing negative thought patterns that go along with pain and make pain worse, Wilson says. It can include relaxation techniques, controlled breathing exercises, music, art, prayer, imagery and numerous other things.
"These are not new things, but there is more recent evidence showing they can be helpful for people," Wilson says.
One randomized clinical trial, published in JAMA Neurology, found that patients with chronic spinal pain experienced reduced pain and improved function using "neuroscience education." Essentially, they were taught how pain works in the nervous system, and they concentrated on functionality in movements, exercising despite the pain. Compared with a group that received a common program of physical therapy and exercises, the neuroscience education group had higher pain thresholds, more reduction in disability and improved physical and mental health.
Wilson's line of research focuses specifically on online pain management tools and tips people can do on their own. One recent study, published in the journal Addictive Behaviors, found that online self-management does, in fact, reduce symptoms for people with pain and opioid use disorders.
Spendlove agrees that these techniques can be helpful.
"I think it's starting to catch on," he says.
MOVING THE NEEDLE
Opiates work by hijacking the endorphin system. It seems counter-intuitive, but the drugs make your brain think you're experiencing a traumatic episode, temporarily stopping the perception of pain.
But the problem is that the body needs increasingly more opiates to achieve the same effect over time. With acupuncture, says local acupuncturist Jacob Godwin, nonaddictive needles can stimulate the same effect as opiates, manipulating your system to reduce pain.
"It's kind of like tricking the brain into doing what the brain might do in a case of traumatic shock," Godwin says.
Godwin says he gets plenty of patients who were on opioids and need to dramatically reduce their dosage. He says a third of the patients at Godwin Acupuncture are veterans. Often, he says, acupuncture proves successful.
The treatment options vary depending on what kind of pain it is. Pain related to a single event from which your body has trouble recovering would be treated differently than, say, arthritis or disc problems. Still, the goal isn't just to manage the pain. Acupuncture treatment can eliminate it over time, Godwin asserts.
He stresses that acupuncture isn't just some magic ancient tradition to treat pain. It's based on science. He says there's a "Hogwarts side" and a "Harvard side" — the latter being real evidence to support acupuncture for pain. Indeed, a study published in the May edition of the Journal of Pain found that acupuncture is effective in treating chronic pain, and that it's not just a placebo effect.
"We know as much about acupuncture for pain as we do about the drugs we use to treat pain... it's very well rooted in science," Godwin says.
RUB IT ON
When it comes to cannabis products like topical cannabidiol oil, Godwin is less sure of the science behind it. "But I know a lot of patients are using cannabis products, edible and topical, and having pretty good results," he says.
Still, right now, much of the evidence for CBD oil is anecdotal. CBD, for those who don't know, contains little to no THC, the chemical compound that makes you high from smoking marijuana. It's legal in many states, with people reporting it can help with things like fibromyalgia, epilepsy and diabetes. A few studies have found that topical CBD oil can help with arthritis pain or multiple sclerosis. One report published in the National Academies of Sciences, Engineering, and Medicine found that adults with chronic pain experienced a "significant reduction" in pain symptoms with CBD oil.
Still, more research needs to be done, Wilson says. She welcomes people to explore and try it for themselves.
"The research is not as robust as we'd like it to be," she says. "It is a definite area of interest."
And there are always other ointments, creams and rubs that can help with pain. Spendlove recommends balms containing lidocaine. There's little risk, he says, other than potential irritation of the skin.
OVER THE COUNTER
And then there are pills. Acetaminophen (Tylenol) and ibuprofen (Motrin or Advil) can both work to treat pain, often more effectively than opioids.
Still, there are some risks with these over-the-counter drugs as well. Anyone with liver disease needs to be careful about using Tylenol, as it can be damaging to the liver. And people with a history of gastric ulcers need to be careful about ibuprofen as well.
"Any medicine in high dose can be potentially dangerous," Wilson says.
Amy Doneen, an associate professor at the WSU College of Medicine and the medical director of the Heart Attack & Stroke Prevention Center, says multiple studies have revealed a significant risk with ibuprofen for patients at risk of stroke or heart attack.
"Long-term use of ibuprofen increases stroke and heart attack risk, which is why we don't put our patients on it," Doneen says.
It's why Doneen recommends other ways to address pain that do not affect blood pressure or kidney or liver health. Unsurprisingly, she mentions mindfulness, acupuncture, physical therapy and other nonmedical ways to manage pain.
"I'm a huge fan of all of it," she says. "It's the whole idea of getting to the root of the pain."
EMERGING TRENDS
A TENS UNIT (transcutaneous electrical nerve stimulation) sends an electrical current through the skin via stick-on electrodes, stimulating nerve pathways to produce a tingling or massaging sensation that decreases the perception of pain. Specifically, it helps with nerve pain. The battery-operated device can be bought for a reasonable price.
Washington State University is also leading a study to understand the relationship between sleep and chronic pain. Marian Wilson, WSU assistant professor, is leading the study, in collaboration with University of Washington's Department of Rehabilitation Medicine. It could help answer several questions: Does pain get worse with less sleep, or does pain cause lack of sleep? Can relaxation techniques alleviate pain?