When Ethan Corporon first pumped a shell into the chamber of a shotgun and began blasting away at a house in northwest Spokane last fall, he had already exhibited many signs of being unstable and violent.
He talked to people who weren’t there and kept a shotgun buried under mulch in his yard in the South Perry neighborhood.
Family members worried, in the weeks prior to the gunfire, about the apparent escalation of the 29-year-old’s mental health troubles.
In this, Corporon was much like Jared Lee Loughner, the man who killed six people Jan. 8 in an apparent assassination attempt against Arizona Congresswoman Gabrielle Giffords, whom he shot in the head in a Tucson Safeway parking lot. (Giffords survived, as did 13 others shot by Loughner.)
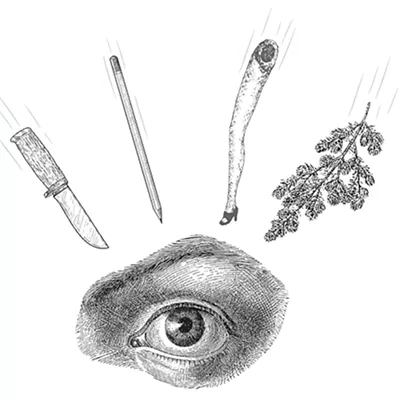
Corporon’s outburst was less lethal. He was the only one to die, and no one else was injured, in a hail of more than 20 police bullets at the busy corner of Monroe and Indiana at mid-afternoon, Nov. 12.
But the two headline-grabbing incidents both involved people who had long exhibited erratic and scary behavior. After a decade of mainstreaming, out-sourcing, downsizing and streamlining, what is the state of mental health care?
It’s fragile, say people in Spokane who strive to juggle ever-present needs with dwindling available funding these last few years. “I’m certainly not hearing a lot of good news from members of our delegation,” says David Panken, CEO of Spokane Mental Health, who spent two days visiting legislators in Olympia in February.
It’s been this way since 2008, at the start of the recession, when Gov. Christine Gregoire said revenue was “pushed off a cliff.” Legally bound to keep a balanced budget — and in a political climate in which tax measures are soundly defeated — Gregoire has cut spending, and cut spending, and cut some more spending.
Over three budget cycles ending this June, one senior state administrator says, reductions in mental health funding will be on the order of $60 million.
Mental health services in Washington took an $18.5 million hit when revenue projections fell short last fall. Gregoire has called for another $17.7 million cut in a proposed supplemental budget for the remainder of fiscal years 2009-2011, which ends June 30. Further, Gregoire wants similar reductions in the next biennial budget for 2011-2013.
Behind The Numbers
In human terms, “We estimate that, if the governor’s proposal goes through, the impact will be about 26,000 fewer people being served in the public mental health system,” says David Dickinson, director of the state’s Division of Behavioral Health and Recovery, an arm of DSHS (the Department of Social and Health Services).
So should we should worry about more Jared Lee Loughners and Ethan Corporons? Well, yes and no, but mostly no.
A wave of media attention followed the Tucson shooting, suggesting that cuts to services may have allowed Loughner to “slip through the cracks” of a once public mental health system lately reduced by budget crises. But as disturbing as Loughner appeared to be — scaring classmates and teachers and attracting the attention of police — mental health professionals interviewed for this story are quick to note he has not yet been diagnosed with any mental illness.
On the other hand, Corporon had previously been institutionalized and, two weeks prior to his death, a sister tried once more to find him help. The two went to Providence Sacred Heart Medical Center, where Ethan Corporon filled out a form that he was seeking help for paranoia and delusions. They waited for hours. Finally, Ethan Corporon met, alone, with a mental health professional.
After a 10-minute meeting, the sister says Ethan told her he was turned away for not having insurance. Hospital officials say his lack of insurance was not a factor, but that Corporon did not meet criteria for in-patient care. He was sent away with a brochure for other programs to check out.
It appears he received no help prior to digging up the shotgun two weeks later.
“Don’t Look Away”
Other instances of people with mental health issues becoming violent or deadly have been shoved into the budget debate.
In early December, Gov. Gregoire called a special session of the Legislature to deal with budget cuts. A health worker’s union, SEIU 1199NW, published a white paper: Don’t Look Away: With a Collapsing Mental Health Safety Net, Washington is Losing the Fight against Preventable Tragedies.
The paper suggested recent high-profile mass killings in Western Washington (including Maurice Clemmons’ ambush-murder of four police officers in a suburban Tacoma coffee shop) all had at their root the failure of the mental health safety net due to various programs being eliminated or reduced.
There was immediate reaction from others in mental health care, scolding the union for sensationalizing the tragedies and for launching a fear-based campaign. Faculty at the University of Washington’s School of Social Work responded in an open letter, noting the “vast majority” of people living with mental illnesses are never violent, and that the reasons for violent acts are complex.
There was some agreement, however, that budget cuts can be harmful.
“A breakdown in the … safety net will be tragic, because people do recover when treatment is available,” the letter summarizes. Fewer services mean more people on the streets or in jails, it says, concluding: “These consequences need to be proclaimed loud and clear, but not by creating a false perception that equates mental illness with the threat of violence.”
Jennifer Stuber argues we have all missed the real point of Tucson. An assistant professor in the UW School of Social Work, she has formed a coalition that encourages better media reporting on mental health issues (mentalhealthreporting. org).
In a post-Tucson essay, she writes, “When Jared Loughner’s behavior deviated from the norm, he was shunned and rejected by his college, local employers, acquaintances and friends. In short, his community did not care or did not know how to deal with him.”
In other words, by coming across as erratic and weird — showing signs he needed help — Loughner’s behavior made the rest of us uncomfortable, we shied away and he was never offered the help he needed.
Cuts to the safety net were not a factor, Stuber argues.
Mental health professionals in Spokane echo the sentiment that people with mental illnesses are very rarely violent, but they also decry the budget cuts.
Just as in the letter from the UW social work faculty, they see clients losing shelter or medication or counseling, and winding up on the streets where they can be preyed upon, or can wind up in jail. If they are jailed for 30 days or more, they face a further setback of losing federal Medicaid eligibility. The benefits can be restored by reapplying, but the process can be difficult to navigate.
What’s at Risk?
“The reason we are so concerned about significance of this cut, is those funds are utilized principally for crisis services, residential services, and any service we can provide to people who need intensive care but who don’t have Medicaid,” says Panken of Spokane Mental Health. “We are primarily a Medicaid system.”
Both the House and Senate released proposed supplemental budgets in February with mental health reductions that are less drastic than the governor’s $17.7 million. Each would cut $12.5 million, though they arrive at that total by different routes.
Within those supplemental budgets, Panken says, are provisions for programs that help Spokane divert people out of hospital emergency rooms and into various in-patient programs, such as group homes, psychological counseling or crisis services.
The proposed Senate budget keeps the current funding intact at $1.5 million. The House cuts it in half.
The uncertainty of which programs are about to be chopped is nerve-wracking, says Dickinson, the director of Behavioral Health and Recovery. The cuts will be painful, wherever they land.
“Last year we served about 144,000 people, so [service reduction] would be significant. And what it means in some cases, when you really boil it down, is that folks who are in crisis may not get crisis services. They may show up in emergency rooms of hospitals or in county jail systems.
“We live in an interconnected world, and cuts in one area have impact in others. This puts additional pressure on Eastern State Hospital,” Dickinson says.
Eastern State Hospital is recognized, if only by geographic isolation, as playing a critical role in the crisis service net for the RSNs (Regional Service Networks) that serve the 21 Eastern Washington counties. The hospital provides long-term care that is pretty hard to replace.
As such, it shields Spokane County from the worst of the budget cuts.
“As far as impact in the budget, we have been very fortunate,” says Christine Barada, director of Spokane County Community Services, the RSN that disburses mental health care funding to agencies and contractors here.
“Our county commissioners and our legislators have worked very hard, and there is an understanding that with Eastern State Hospital in our region, and being a health-care service Mecca, this area really needs funds to divert people from hospitalization and to keep them in the community,” Barada says.
The trouble is, she notes, the successive rounds of budget reductions have lessened the number of beds available at Eastern State. It’s been like the slow leak of air out of a tire.
“A couple of years ago we were allowed 101 beds at Eastern before we were charged a fee. Now it’s 85,” Barada says.
And the beds are rarely empty.
John Wiley, a spokesman for DSHS, says that 280 of the 287 beds at Eastern State Hospital were filled in February. In addition, Wiley says, “We average over 100 admissions a month.”
For each bed over the first 85, the RSN now pays a fee that comes out of the money available to help people who don’t have Medicaid coupons.
“We mainly are a Medicaid-only state … [but] a lot of people out there don’t have a Medicaid coupon, and there is no place for them to go,” says Marilyn Wilson, clinical director for Spokane Mental Health.
“Our crisis department will see anybody. But to get enrolled in services, if you don’t have the right funding, there is not much for you,” Wilson says.
Scrambling for Help
People seeking mental health services in Spokane are being squeezed from all sides, we are told. The Disability Lifeline (formerly known as general assistance — unemployable) is being reduced from an already Spartan $359 a month to $257, Wilson says.
“A lot of these people have a mental illness. This will make it difficult to fi nd safe, affordable housing and to pay rent,” Wilson says.
The available funding to help people who don’t qualify for Medicaid has been under such stress in the budget squeezes that fewer dollars are available for crisis services or in-patient care for these folks, Barada says.
For Spokane Mental Health, the CEO Panken says, affected services include psychiatric treatment for voluntary and involuntary patients at in-patient facilities, as well as support for crisis teams that help children and adolescents as well as adults.
The result?
“Cost-shifting,” Wilson says. “Many more [patients] will be in hospital emergency departments, or dealing with police and fire and certainly the jail. And there will be more people on the street without services of any kind.”
Dental services have already been cut in January, she says. “When people have a toothache, now they go to the emergency room. People have to go somewhere for services,” Wilson says.
The upshot is, “… a greater cost to the community and a greater risk to clients,” Wilson says.
The cuts for vulnerable locals — often poor, many unemployed, and seeking help for mental illness — are frankly awful to deal with, people working with these clients say. “I think people simply aren’t able to speak about it at this point,” Panken says.
Gov. Gregoire herself said of her proposed budget, “It doesn’t reflect my values, and I don’t think it reflects the values of folks across the state.”
“She more or less disowned it, didn’t she?” Panken says. “She has to propose a balanced budget, and she used it as a wakeup call.”
The New York Times reported, in the wake of the Tucson shootings, that Arizona Gov. Jan Brewer is proposing cuts in eligibility for Medicaid. Gregoire has already reduced Medicaid payment rates to providers.
The National Association of State Mental Health Program Directors estimates, according to the Times, that some $2.1 billion has been cut from state mental health budgets in the last three fiscal years.
When it comes to further restricting access to Medicaid, Panken says, “It doesn’t make a lot of sense to cut a dollar that brings in another dollar,” from the federal government.
In North Idaho, too, cuts to Medicaid funding for the mentally ill and developmentally disabled are expected.
“If we ignore any health-related concern that’s not insured or funded it will cost all of us more, ultimately,” Panken says. “It will cost hospitals more.”
Mike McMurtry, of SL Start, runs a program that helps people with disabilities — including mental and developmental disabilities — find jobs.
He, like many others, is closely tracking the budget proposals in Olympia: “Almost every day I get an updated budget from somebody.”
McMurtry says that when funding is cut, his clients scrimp like we all do. But in their cases, they may decide to quit the prescription drugs they need to function. As a result, they may drop from the programs, or perhaps lose jobs or have trouble staying in apartments.
This not only has a human cost, but a societal one, he says. While economists and politicians bemoan the 9.4 percent unemployment rate, the rate for people with disabilities, “is easily two times that number. The figure we’ve talked about for years is over 40 percent,” McMurtry says, noting a lack of hard data because, often, “people with disabilities just give up looking.”
It shouldn’t be that way, he says.
“The funny thing is there is scads of proof that shows that the work we do through the programs puts money back into the system. When we put someone to work they come off whatever roll they were on and begin to pay taxes. Studies show a return of $3, $4 or $5 for every $1 that’s put in,” McMurtry says.
“We certainly don’t believe we’re going to go through this [legislative] session and avoid cuts to mental health programs … that’s not realistic,” Spokane Mental Health’s Panken says.
“We know legislators have a difficult job to do. But we are concerned the fabric of public safety [will be] torn so greatly that we can’t do our part to protect the public and treat the vulnerable people who need care and treatment,” he says.
“Certainly, a small portion of any population can be violent, assaultive or aggressive,” Panken says, “But with mental health that is no more so than the general population, often less. These people tend to be victimized,” on the streets, he adds.
Time of Crisis
“Nationally, we have to deal with the mentally ill,” says Spokane Police Chief Anne Kirkpatrick.
Kirkpatrick was recently among 100 people invited to a Harvard University Kennedy School think tank. When the group was quizzed for pressing topics, “I raised my hand and said we need to have a public policy discussion on the future of mental health and how it affects law enforcement,” she says.
Most people with mental illnesses are not violent, the chief says, but when they are, and when they are on the street, they pose risks to themselves and the public.
“I have reinvested my resources to make sure we are committed to crisis-intervention training, but we need to go beyond that,” she says. “Law enforcement is just not the answer” as the fallback for funding cuts and loss of residential beds, she says. “We’ve got to do business a different way.”
Christine Barada, of the county, and Marilyn Wilson of Spokane Mental Health both point out Spokane County Jail is unique in Washington for having its own certified mental health unit.
“We are the only one in the state, and it is very well-received,” Barada says. “It was a lengthy process to establish an actual center in the jail for mental health services and oversight.”
The jail has a doctor, contracts with Spokane Mental Health for psychiatric services and dispenses appropriate medications.
The goal of mental health services in Spokane, even at the jail, is to stabilize people in crisis and to “return them to their homes,” Barada says.
“Safe and affordable housing for the mentally ill is important,” Wilson adds.
So important that many agencies and providers have also become developers, building apartments and other housing stock around the county.
“Mental health funding is like a roller coaster,” Wilson says. “In 2003 or 2005 we had lots of cuts. We had to lay a lot of staff off. There were program cuts. Luckily, we built those back up,” in better budget years, she notes.
What of Ethan Corporon, who knocked on the door of the mental health system and was turned away? It appears he took the correct initial step.
“Individuals who feel they are a danger to themselves, they first generally go to Providence Sacred Heart hospital for stabilization and to determine if either changing medications or starting medications may be helpful,” Barada says.
In fact, Providence Sacred Heart is the only hospital in the region that even admits mental health patients. It may be, Barada says, that Corporon didn’t say — or that the intake staffer didn’t catch — that he was in dire need of help.
Budget cuts or no, she says, “We have a requirement to serve all people in crisis.”